Carbohydrates are essential nutrients, that not only serve as an important fuel to meet the body’s metabolic demands, but also play an important part in the digestive process. The fibre present in plant foods consists of carbohydrates known as NSP (non starch polysaccharides) which play an important part in the movement and absorption of nutrients in the intestines. For centuries it was thought that protein-rich foods supplied the body with the optimum fuel to maintain strength and stamina, and this concept is still entrenched to some extent to this day. Increasingly, however, carbohydrates are coming into their own as the fuel which keeps us functioning optimally, and it is now common knowledge that carbohydrates are the preferred energy source utilized by the body..
It has been known for some time that communities that subsist largely on high-carbohydrate diets are notable for their stamina and excellent health. One such group is the Tarahumara Indians of Mexico, whose chiefly vegetarian diet consists of 75-80% carbohydrates. Moreover, degenerative conditions such as hypertension, obesity and age-related cholesterol level increases are virtually absent from the tribe.1,2 The stamina of the Tarahumara Indians is well demonstrated in their most popular sport which is raripuri, where participants race for 150-300 km kicking a wooden ball.3 Achievements like these have challenged the “proteins for energy” concept and have encouraged an entire new investigation into the role of primary nutrients in human nutrition.
Scientific endeavours to enhance athletic and other performances have done much to explode the proteins for energy myth. In ancient times the Greek athletes consumed large amounts of meat before athletic events,4 but today it is acknowledged that vegetarian, high-carbohydrate diets, are superior to high-protein diets when it comes to enhancing stamina and endurance. Indeed, “carboloading” (increased carbohydrate intake) is extensively practised when preparing for sporting events. Improving the carbohydrate intake in athletes increases the quantity of glycogen which is stored in the muscles and this in turn improves the athlete’s performance by delaying fatigue.5 Training depletes the glycogen reserves in the muscles, but a high-carbohydrate intake rapidly replenishes these reserves, whereas this is not the case if a low-carbohydrate diet is followed (Fig.2.1).

Figure 2.1. Reduction in muscle glycogen during several days of intense training. (From ref. 6)
To enhance glycogen turnover, especially in athletes, a diet consisting of 65-70% carbohydrates has been suggested (550-650g/day),7 but few athletes consume such diets simply because modern eating habits do not cater for such high-carbohydrate intakes. It has, in fact been found that carbohydrate intakes for most male endurance athletes range from 40% to 55% of total calories consumed, whereas other athletes engaged in other sports consume even lower levels of carbohydrates. To assist athletes in improving their carbohydrate intake, extensive guidelines have been developed, which list the foods with a high-carbohydrate content.5 Many of the high-carbohydrate foods in these lists are, however, refined foods and sweets, which cannot be considered as healthy.
The value of NSP (fibre) together with certain starches that are resistant to digestion in the small intestine, is now being discovered, and highly refined foods cannot meet the criteria required for healthful living. A new concept of nutrition is necessary which takes us away from modern highly refined foods and at the same time supplies primary nutrients in proper ratios. Only whole foods can supply this optimum relationship between nutrients, and will not only be of benefit to the athlete, but to every human being. Whole foods will also be of benefit to overweight individuals without being unduly restrictive in terms of the quantities of food which may be consumed. Athletes burn up more energy than non-athletes, but the ratio of nutrients required by both should remain roughly the same. For the general public, a minimum energy intake of 1 200 kcal is advised, and for athletes 1 600 kcal8 (for a more detailed discussion of caloric needs see chapter 5), and a whole-food programme can certainly supply this. Fear is often expressed that a high-carbohydrate diet would be restrictive in terms of the amount of protein that is then available, but this fear is unfounded if a varied diet is followed which makes allowances for essential amino acid variations in foods, as was discussed in Chapter 1. Moreover, recent evidence indicates that high-carbohydrate intakes can, without increasing protein intake, improve protein retention and synthesis.9
Carbohydrates in food
Carbohydrates are manufactured in plants by the process of photosynthesis using carbon dioxide and sunlight. As animal products contain virtually no carbohydrates, fruits, vegetables, grains and legumes are the main carbohydrate foods. Moreover, each of these plant foods supplies a different variety of carbohydrates, and it is therefore advisable that we know something about the structure and assimilation of carbohydrates in order to utilize these foods to our advantage. The carbohydrates in plants are largely constructed of various combinations of five simple sugars known as monosaccharides of which glucose forms the principle fuel of our bodies. The glucose molecule can have more than one configuration (Fig. 2.2), and when strung together to form polysaccharides, the properties of these macromolecules will be influenced by the type of glucose molecule incorporated.
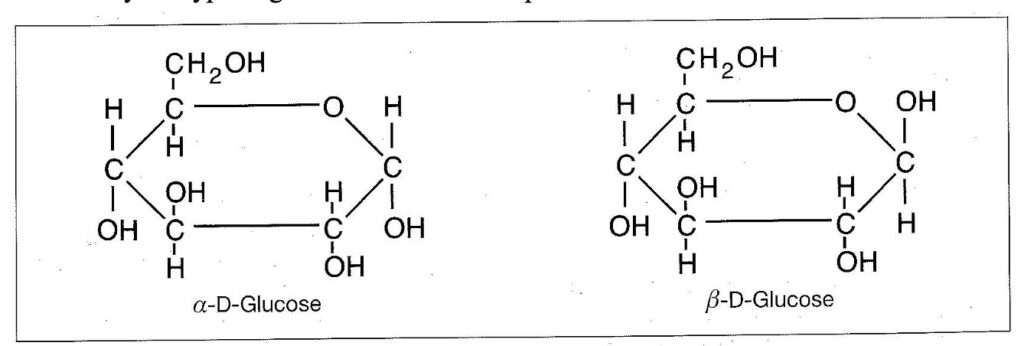
Figure 2.2 The structure of α- and β -D-Glucose
Although α- and β-D-glucose appear very similar in structure, they are different in their biochemical properties. Whereas β-D-glucose occurs in cellulose which is a non-soluble fibre, α-D-glucose occurs in starch which is the most common storage material of plants. Starches are polysaccharides made up by numerous glucose molecules linked together in chains and stored as granules in various plant tissues. Not all starches are equally digestible in view of differences in stereochemistry and, whilst readily digestible starches form the main energy supply for the body (or they should form the main energy supply), starches that are resistant to digestion play an important role in the maintenance of colonic bacteria. Humans cannot digest cellulose as we lack the enzyme cellulase, but these fibres also play an important part in digestion, as they add bulk and improve gut motility. The structure of starch and cellulose is presented in figure 2.3.

Figure 2.3. The structure of starch and cellulose.
Starch is broken down to glucose by digestive enzymes, and besides glucose, there are other important monosaccharides which play a significant role in human nutrition. Fructose is the monosaccharide found mainly in fruits and some other plant foods, and galactose is a component of lactose the disaccharide found in milk. Galactose is also found in some of the storage carbohydrates of legumes and other seeds. A disaccharide consists of two simple sugars bound together. Another disaccharide that plays a significant role in human nutrition is sucrose (common table sugar), which is a combination of fructose and glucose. The structures of these molecules are presented in figures 2.4 and 2.5.

Figure 2.4. The structure of fructose and galactose.

Figure 2.5. The structure of sucrose and lactose.
Digestion of carbohydrates
In natural foods the primary nutrients come prepacked with a variety of vitamins and minerals, which enhance the maximal utilization of these foods. Whole foods contain fibres which influence the rate at which food passes through the intestine, and also control the rate at which the digestive products are absorbed. Moreover, the vitamins and minerals found in whole foods play an essential role in metabolizing the nutrients we eat. Unfortunately today’s society chooses rather to eat refined foods which are poor in vitamins, and the lack must be supplied from the body’s reserves, thus robbing the body of these essential components. Eating carbohydrates only in the refined state can eventually lead to numerous deficiency diseases.
The enzymes which digest carbohydrates can be divided into two categories, the
polysaccharidases and glycosidases. The former hydrolyse the long chain carbohydrates such
as glycogen and starch, whilst the latter act on disaccharides such as sucrose, fructose, maltose and lactose thus breaking them down into their constituent monosaccharides for absorption. The most common polysaccharidases are the amylases (ptyalin and amylase) which are secreted by the salivary glands and the pancreas. Cellulase, is a polysaccharidase produced by symbiotic micro-organisms in the gut of cellulose-utilizing animals such as cattle, sheep, and termites but humans cannot digest cellulose. Cellulose is, however, a natural fibre which supplies bulk and ensures easy passage of ingested material through the digestive tract.
Carbohydrate digestion is first initiated in the mouth, and it is, therefore, essential that food be chewed adequately to allow this process to take its course. The enzyme ptyalin occurs in saliva and it converts the starch found mainly in vegetables, grains and legumes into the disaccharide maltose. Ptyalin is inactivated below pH4 so that starch digestion will cease in the stomach if the pH drops below this level. The digestion of starch will continue in the stomach as long as the pH does not drop below pH4. Concentrated protein foods such as animal products will quickly induce a pH drop and consequently prevent further digestion of starch in the stomach. Proteins found in grains and legumes do not, however, require an excessive acid medium for digestion and are thus ideal companions for fruits or vegetables. Nuts are also an excellent source of protein but should be eaten in moderation, because excessive intake will also lower the pH in the stomach.
When food passes from the stomach into the duodenum, the environment again becomes alkaline and favours the digestion of carbohydrates. In the duodenum the enzyme amylase, which is released by the pancreas, will continue with the break-down of starch to maltose which in turn is acted upon by the intestinal glycosidase maltase which breaks down maltose to glucose. The glucose is then absorbed and conveyed to the liver where it is stored in the form of glycogen. Glycogen is also stored in the muscles and thus acts as an energy reservoir, and when required it will be converted to glucose again. Resistant starches and soluble and insoluble fibres reach the large bowel undigested, and some of these components are then broken down by colonic bacteria.
Diet and control of glucose levels
The body needs a constant supply of glucose, not only because it is an important energy source, but because certain tissues such as the brain and nerves cannot function without it. For this reason glucose levels are precisely controlled by the two hormones glucagon and insulin. Insulin is produced by the islets of Langerhans of the pancreas, and its function is to lower blood glucose levels by stimulating the conversion of glucose to a storable form of energy such as fat. The hormone glucagon has the opposite effect and increases the glucose levels. The ailment diabetes mellitus results from a lack of insulin production, whereas excessive insulin production results in hypoglycaemia or low blood sugar. Rapid uptake of glucose can be brought about by a refined food diet and can lead to hypoglycaemia or, in the case of the diabetic, it can be brought about as a result of an insulin injection.
Monosaccharides such as glucose, fructose and galactose require no digestion and are absorbed as is. The disaccharides, such as sucrose, are rapidly converted by the glycosidases in the intestine and it is easy to flood the system with glucose if refined foods are consumed. The subsequent glucose surge will lead to extensive insulin production, and because the glucose will then be converted to fat and glycogen, the blood sugar levels will be lowered more than normal, thus leading to hypoglycaemia. Hypoglycaemia initiates a series of bodily responses and the reduced glucose levels are recognized by the brain, which in turn triggers a response by the sympathetic nervous system. Adrenalin and other hormones are then released to counteract the fall in glucose levels, and this manifests itself in numerous symptoms of which only a few
will be discussed here.
Symptoms of hypoglycaemia
These symptoms can be divided into two categories, namely: autonomic activation and
neuroglycopenic symptoms as summarised in table 2.1.
| SYMPTOMS OF HYPOGLYCAEMIA | |
| Autonomic activation | Neuroglycopenic |
| sweating (even heavy sweating), shaking, warmness, pounding heart and increased heart rate, anxiety and shivering. | confusion, drowsiness, weakness, difficulty in speaking, loss of concentration, visual disturbances such as double vision and dizziness. |
Table 2.1. Symptoms associated with hypoglycaemia. (From reference 10)
Many of these symptoms can manifest themselves at night or early in the morning, in view of the abstinence from food during this time, and therefore insomnia, fear and even hallucinations can be additional symptoms. The normal range of blood glucose levels should be between 80-120 mg/100ml in the morning before a good meal. After a meal, the blood sugar level will rise but should drop to this range within a few hours. Unfortunately, modern lifestyles can have a detrimental effect on the maintenance of normal blood sugar levels, and refined foods and certain stimulants are some of the main culprits.
Refined foods are used extensively in the food industry, and many processed foods as well as the myriads of sweets, cookies and soft drinks on the market contain large amounts of hidden sugars, mostly in the form of sucrose. When these foods are consumed, most of the sucrose will rapidly be converted to glucose and fructose, thus causing a glucose surge. Some of the sucrose will even enter the bloodstream unaltered and will be treated as a foreign substance as there are no enzymes to break it down outside the intestinal tract. Moreover, caffeine, which is found in tea, coffee and many soft drinks, as well as theobromine that is found in cocoa and cocoa products such as chocolates, also induce hypoglycaemia as they stimulate the conversion of stored glycogen to glucose which in turn leads to insulin release and subsequent hypoglycaemia.
The modern trend to drink large amounts of soft drinks, can prove particularly hazardous, as these contain very high levels of sugars. Although soft drink firms add only sucrose to their drinks, these beverages also contain large amounts of glucose and fructose. This anomaly is brought about by the high acidity of these drinks, which encourages acid hydrolysis of sucrose. As both glucose and fructose are less sweet than sucrose, the companies compensate for this by adding more sucrose, and an average carbonated beverage can contain as much as 136g/l of sugar11 which is more than ten teaspoons of sugar per 340ml can.
Avoidance of high sugar drinks, caffeine and theobromine together with the consumption of whole foods such as unrefined grains, legumes, fruits and vegetables will prevent hypoglycaemia. The presence of soluble fibre in these foods ensures a slow release of simple sugars over a period of time, thus preventing the glucose surge associated with refined foods. Surge releases of insulin will also be avoided and in addition the whole foods come prepacked
with the essential vitamins (particularly the B-group) and minerals required for their effective metabolism. People suffering from hypoglycaemia should also include more of the high energy whole foods, such as unrefined grains and legumes in their diet, because oats and bean products contain high levels of soluble fibres which offer protection against hypoglycaemia. It is not necessary to give up one’s sweet tooth, but one should encourage the use of naturally sweet foods, such as dates and raisins as sweeteners, and avoid large amounts of refined sweeteners which consist largely of empty calories. In table 2.2. the chemical composition of some of the most common sweeteners, as well as foods with added sugar, is presented.

Table 2.2 The composition of selected sweet foods, drinks and sweeteners. The figures are for 100g portions. (Adapted from reference 12)
It is noteworthy that none of these sweet foods contain any appreciable amounts of fibre, and they are also vitamin poor. If these items are to be used, they should be used sparingly and preferably in conjunction with foods rich in soluble fibres such as fruits, grains and legumes. It should also be noted that brown sugar, molasses, honey and jams do at least contain some vitamins and minerals, whereas the refined products do not. In most countries in the Western world the consumption of sugar is somewhat above 100g/person/day or more than 15% of the daily caloric intake.13 Obviously, this is far too high, and in view of the problems associated with such a high sugar intake there has been a move away from sucrose in certain health circles, and consumption of fructose is recommended in the place of sucrose. Fructose is often considered to be the perfect substitute for sucrose as it is natural fruit sugar. Pure fructose is, however, also a refined sugar and can cause similar conditions as sucrose.
Fructose consumption does not lead to as high postprandial glucose surges as does the consumption of sucrose, and so it does seem to have some advantages over the consumption of sucrose. It does, however, lead to increases in LDL cholesterol levels, and some researchers have also found that it will increase the levels of triglycerides.14,15 Fructose loads will also induce hypoglycaemia because fructose facilitates the formation of glycogen.13 These facts once again underline the principle that refined foods, in whatever form, are not the most wholesome of foods and should be used in moderation. It is therefore advisable to cultivate the habit of substituting whole-food sweeteners for refined sweeteners wherever possible.
NSP (fibre) and digestion resistant starch
The importance of fibre in the diet is being recognized more and more. The concept that fibre could play a preventive role in colon cancer was first proposed in 1971 when Burkitt put forth the proposal that fibre could prevent colon cancer by regulating the speed and bulk of the food that passes through the intestines.16 Since that time many studies have shown this hypothesis to be true.17 Whole grain consumption in particular, was found to be inversely correlated to the prevalence of colon cancer.18 Vegetable fibre was also shown to offer protection, and the NCI (National Cancer Institute of the US) has therefore recommended that a variety of foods such as whole grains, vegetables and fruits be eaten rather than fibre supplements, and that dietary fibre levels should at least be doubled over current consumption levels of 10-15g fibre/day.19 Fibre consumption is so low in industrialized countries, because of the excessive consumption of refined foods. Modern grain mills, for example, separate the natural fibres and wheatgerm
from the wheat, thus stripping the wheat of its natural fibre. The bran of wheat is rich in NSP (non starch polysaccharides or fibre) which provides bulk and aids intestinal motility. Furthermore, these outer layers of wheat include the aleurone layers which contain the B-complex vitamins, phosphorus, iron, and proteins in balanced proportions. The wheatgerm is rich in thiamin (vitamin B1) which is essential for carbohydrate metabolism and the natural antioxidant vitamin E. Vitamin E comes prepacked with the polyunsaturated oils in the wheat-germ and thus offers a natural protection against the formation of free radicals when these essential oils are ingested. Whole grains or unrefined grain products such as stone-ground flour, are thus vastly superior to refined products in terms of their overall composition.
The addition of unground wheat berries or broken pieces of grain to the flour is also a poor way of adding fibre to grain products. These hard pieces pass through the intestines largely undigested, add little bulk and can even damage the delicate epithelia on their way. They do not aid in water retention in the stools and do not provide a large enough surface area for the elimination of wastes. Flour used for bread-making should be thoroughly ground and if whole grains are used for the preparation of porridges, then they must be well soaked or/and thoroughly cooked, as raw grains contain enzyme suppressants which interfere with the digestive process. Cooking or sprouting destroys these suppressants and thus allows for maximal utilization of the nutrients in the grains.
As fibre content in the diet increases, bowel transit time decreases and faeces weight and the number of defecations increase.20,21 Furthermore, the consistency of the stool is far softer on a natural high-fibre diet than on a low-fibre diet thus eliminating constipation and its secondary effects such as colitis, appendicitis, diverticulosis, and hiatus hernia. Oats and bean products contain large quantities of water-soluble fibre and are particularly efficient in reducing blood cholesterol levels, particularly LDL-cholesterol, which is the variety which tends to clog blood vessels. 22,23,24,25,26 It was found that the inclusion of oat-bran and beans in the diet decreased LDL-cholesterol concentrations by 23% and 24% respectively in a study done on 20 hypercholesterolaemic adult males.22 Added bran is not nearly as efficient in eliminating cholesterol as is the fibre in whole cereals,27 thus emphasizing the importance of the consumption of whole, unrefined foods as means of controlling cholesterol levels. Some studies suggest that oat bran acts as a placebo,28,29 but other studies have shown that this conclusion is probably unfounded.30 By binding cholesterol and bile acids, fibre not only reduces cholesterol levels but also protects against colon cancer, as secondary bile acids, which are formed by bacterial conversion of bile acids, are carcinogenic.31 The relationship between the incidence of colon cancer and fibre intake is presented in Figure 2.6.

Figure 2.6 Average regional NSP intake in relation to age standardized colon cancer death rates 1969-1973 in Great Britain. (Adapted from reference 32)
Wheat-bran was also found to lower the concentrations of oestrogens in women, particularly serum oestrogen and oestradiol.33 The presence of free and albumen-bound oestradiol has been associated with an increased risk of breast cancer,34 and the bran can thus offer protection against this form of cancer. Precisely how fibre affords protection against this form of cancer is uncertain. When dealing with fibre, it is important to note that there are two categories of fibre, and these two differ in their function.
Water-insoluble fibres
Water-insoluble fibres include such fibres as cellulose, lignin and certain hemicelluloses. These fibres have a considerable effect on stool size and the time that the ingested food stays in the digestive tract, but they have little or no effect on intermediary metabolism,35,36 or the growth of the bacterial population in the colon.37 The bulking effect of water-insoluble fibre on the intestinal contents, however, dilutes the concentration of substances that can cause cancer and this type of fibre also ensures rapid elimination of harmful cancer promoters in the colon. Most studies confirm that water insoluble fibre has a protective effect against chemical carcinogenesis, and both bran and cellulose were effective in reducing the number of tumors formed under chemically induced carcinogenesis.38
Refined food leads to constipation, but on a high natural fibre diet stools will not only be softer, but will be passed more frequently. Two to three stools a day are consistent with healthy bowel movements, whereas one stool or even fewer per day may be categorizes as constipation. This might seem excessive to those who pass stools only once a day or even less frequently. If we, however, consider that most people consume two to three meals per day, then it is only logical to eliminate the waste material more than once a day. Waste products that remain in the colon for lengthy periods of time will be acted upon by the colonic bacteria and converted to potential carcinogens. Furthermore, the compaction and pressure required to eliminate fibre-poor stools can produce diverticulosis of the intestinal tract (small pouches), and hardened portions of faeces can become trapped, thus eventually causing inflammation as in the case of appendicitis. Moreover, the increased abdominal pressure required to eliminate hard stools can also produce hernias and will force more blood from the large abdominal vessels into the femoral vessels thus causing varicose veins. Considering the high fibre content of whole-plant foods, it is thus not surprising that diverticulosis is less common in vegetarians than in omnivores.39 There is a strong inverse association between high stool weight and colorectal cancer.40 As there is a linear relationship between stool weight and NSP consumption (5g increase in stool weight for every 1g NSP consumed), both the WHO and the UK department of health have recommended an average daily intake of 18g NSP.41,38.
Water-soluble fibres and resistant starch
In contrast to the insoluble fibres, water-soluble fibres have little effect on stool size, transit time and mineral absorption, but they do have an important effect on secondary metabolism. As noted previously, resistant starch is starch that resists digestion in the small intestine because of the different stereochemistry of these starches. All starchy foods such as grains, legumes and starchy vegetables such as potatoes contain resistant starch. Even fruits, such as bananas that are still slightly green, contain resistant starch. When soluble fibre and resistant starch enter the colon, they are fermented anaerobically to produce short chain fatty acids (SCFA), acetate, propionate, and butyrate as well as gas. Moreover, bacterial growth is enhanced which, together with water binding to residual unfermented NSP leads to increased stool weight, dilution of colonic contents and faster transit time through the large gut.38 This in turn reduces the time that potentially harmful substances can come into contact with mucosal cells.
The SCFA which are produced in the colon during the fermentation process, are absorbed by the intestinal mucosa thus enhancing the functional capacity of the epithelium. Butyrate is also used by the cells in the colon, and because butyrate is formed most efficiently from resistant starch, this type of starch must be considered the prime source of this compound. Butyrate has been suggested as a protective agent against colon cancer,38 and consumption of whole foods rich in complex carbohydrates thus offers protection against cancer in more ways than one.
Diets rich in grains, legumes, fruits and vegetables are thus optimal for maintaining a healthy digestive system.
The water-soluble fibres include such fibres as pectin, hemicelluloses, and storage polysaccharides that are found mainly in fruits and vegetables, and gums which are found mainly in cereals. As the bacteria in the colon break down a large proportion of these water-soluble fibres, they do not contribute to faecal bulk as do non-soluble fibres. Besides contributing fermentation products, for use by the mucosal cell of the colon, soluble fibres are known to lower cholesterol levels and to prevent the postprandial (after meal) glucose surge and subsequent hypoglycaemia associated with a refined food diet. Once again, it is the fruits, vegetables, legumes and grains which contain soluble fibres which can retard the rate of glucose absorption. In the case of fruits, the soluble fibre which retards the rate of glucose absorption is pectin, and it prevents the glucose surge and subsequent hypoglycaemia associated with a refined food diet devoid of natural fibre.42 The same effect is achieved by soluble fibres found in oat bran, and has been attributed to the presence of the oat gum β-glucan. This polysaccharides occurs in commercial rolled oats and is highly viscous. It has been found that the inclusion of oat gum in a meal containing glucose, significantly reduced the postprandial glucose and insulin surge that occurs in glucose meals that do not contain the oat gum (Figure 2.7).43
In figure 2.7 it can be seen that the glucose meal by itself produces a large increase in plasma glucose levels which is accompanied by a surge release of insulin. The result is that glucose levels rapidly drop and even drop below the fasting level (indicated by the zero in fig. 2.7), thus producing a hypoglycaemic condition. Soluble fibres probably prevent the glucose and insulin surge by slowing the rate of glucose absorption44 and by slowing the rate at which the enzyme amylase digests the foods containing the viscous fibres.45 This allows for a longer period of time over which glucose is absorbed, particularly as soluble fibres also slow down the rate at which glucose is absorbed across the wall of the intestine.46 It is through the combination of these mechanisms, that soluble fibre affords protection against hypoglycaemia.
An argument which is often levelled against a fibre-rich diet, is that it will inhibit the uptake of minerals and other essential nutrients. In a recent study it was, however, found that the higher fibre intake of vegetarians did not affect mineral utilization adversely, and depending on the variety in the diet, the uptake of magnesium, iron, copper and manganese could actually be enhanced.47 A varied whole food diet rich in carbohydrates will therefore afford the highest protection against degenerate diseases, as well as supplying all the body’s energy, mineral and vitamin needs.

Figure 2.7. Postprandial changes in plasma glucose and insulin levels after a 50g glucose drink (dots) and a glucose plus oat gum drink (squares). Adapted from reference 43.
REFERENCES
- Conner, W.E., Cerqueira, M.T. Connor, R.W., Wallace, R.B., Malinow, M.R., Casdorph,
H.R. 1978. The plasma lipids, lipoproteins, and diet of the Tarahumara Indians of Mexico.
Am.J.Clin.Nutr. 31:1131-42
- Balke, B., Snow, C. 1965. Anthropological and physiological observation on Tarahumara endurance runners. A.J.Phys.Anthropol 23: 293-301.
- Nieman, D.C. 1988. Vegetarian dietary practices and endurance performance.
Am.J.Clin.Nutr. 48: 754-61.
- Ryan, A.J. 1981. Anabolic steroids are fool’s gold. Fed.Proc. 40:2682.
- Moses, K., Manore, M.M. 1991. Development and testing of a carbohydrate monitoring tool for athletes. J.Am.Diet.Assoc. 91:962-965.
- Costill, D.L., Miller, J.M. 1980. Nutrition for endurance sports: carbohydrate and fluid balance. Int.J.Sports.Med 1:2-14.
- Costill, D.L. 1988. Carbohydrates for exercise: dietary demands for optimum performance.
Int.J.Sports Med. 9:1-18.
- Hoffman, C.J. and Coleman, E. 1991. An eating plan and update on recommended dietary practices for the endurance athlete. J.Am.Diet.Assoc. 91:325-330.
- Welle, S., Mathews, D.E., Campbell, R.G., Sreekumaran, N. 1989. Stimulation of protein turnover by carbohydrate overfeeding in men. Am.J.Physiol. 257:E413-E417.
- Patrick, AW, Bodger, CW., Tieszen, K.L., White, M.C., Williams, G. 1991. Human insulin awareness of acute hypoglycaemic symptoms in insulin-dependent diabetes. Lancet 338:528-532.
- Van der Horst, G., Wesso, I., Burger, A.P., Dietrich, D.L.L. Grobler, S.R. 1984. Chemical analysis of cooldrinks and pure fruit juices – some clinical implications. S.Afr.Med.J. 66:755-758.
- NRIND. 1986. Food composition tables. 2nd ed. South African Medical Research Council.
- Sestoft, L. 1983. Fructose and health. Nutrition Update 1:39-54.
- Hallfrish, J., Reiser, S. Prather, E.S. 1983. Blood lipid distribution of hyperinsulinemic men consuming three levels of fructose. Am.J.Clin.Nutr. 37:740-8.
- Swanson, J.E. Laine, D. Thomas, W., Bantle, J.P. 1992. Metabolic effects of dietary fructose in healthy subjects. Am.J.Clin.Nutr. 55:851-6.
- Burkitt, D.P. 1971. The Epidemiology of cancer of the colon and rectum. Cancer. 28: 3-13.
- Greenwald, P., Lanza, E., Eddy, G. 1978. Dietary fibre in the reduction of colon cancer risk. J. Am. Diet Assoc. 87:1178-88.
- Reddy, B.S.1982. Dietary fibre and colon carcinogenesis: A critical review. In Vahoung,G.V.; Kritchesky, D., eds. Dietary fibre in health and disease. New York: Plenum Press.265-85.
- Butrum, R.R., Clifford, C.K., Lanza, E. 1988. NCI dietary guidelines: Rationale.
Am.J.Clin.Nutr. 48:888-95.
- Beyer, P.L., Flynn, M.A. 1978. Effects of high-and low-fibre diets on human faeces.
J.Am.Diet.Assoc. 72 : 271-7.
- Eastwood, M.A., Elton, R.A., Smith, J.H. 1986. Long-term effects of white meal bread on stool weight, transit time, faecal bile acids, fats and neutral sterols. Am.J.Clin.Nutr. 43:343-9.
- Anderson, J.W., Gustafson, N.J. 1988. Hypocholestrolemic effects of oat and bean products. Am.J.Clin.Nutr. 48:749-53.
- Anderson, J.W., Chen, W.J.L. 1986. Plant fibre: diabetes and obesity. Am.J.Gastroenterol.
81:898-906.
- Gold, K.V., Davidson, D.M. 1988. Oat bran as a cholesterol reducing dietary adjunct in a
young healthy population. Western.J.Med.148:299-302.
- Keenan, J.M., Wenz, J.B., Huang, Z., Myers, S.R. 1990. A randomized controlled trial of oat bran cereal for hypercholesterolemia. Arteriosclerosis 10:873a.
- Anderson, J.W., Spencer, D.B., Hamilton,C.C. et al. 1990. Oat bran cereal lowers serum total and LDL cholesterol in hypercholesterolemic men. Am.J.Clin.Nutr. 52:495-499.
- Burkitt, D.P 1975 Refined Carbohydrate foods and disease. Academic Press P 341.
- Demark-Wahnefried, W., Bowering, J., Cohen, P.S. 1990. Reduced serum cholesterol with dietary change using fat-modified and oat bran supplemented diets. J.Am.Diet.Assoc. 90:223-229.
- Swain, J.F., Rouse, I.L. 1990. Comparison of the effect of oat bran and low-fibre wheat on serum lipoprotein levels and blood pressure. N.Engl.J.Med. 332:147-152.
- Grant, K.I. 1991. Oat bran-panacea or placebo? S.Afr.Med.J.(in press)
- Nair. P.P. 1988. Role of bile acids and neutral sterols in carcinogenesis. Am.J.Clin.Nutr. 48: 768-74.
- Bingham, S.; Williams, D.R.R.; Cummings, J.H. 1985. Dietary fibre consumption in Britain: New estimates and their relation to large bowel cancer mortality. Br J cancer. 52: 399-402.
- Rose, D.P., Golman, M., Conolly, J.M. and Strong, L.E. 1991. High fibre diet reduces serum estrogen concentrations in premenopausal women. Am.J.Clin.Nutr. 54(3):
- Jones, L.A., Ota, D.M., Jackson, G.A. et al. 1987. Bioavailability of estradiol as a marker for breast cancer risk assessment. Cancer.Res. 47:5224-9.
- Munoz, J. 1984. Fibre and diabetes. Diabetes care. 7:297-8.
- Crapo, P.A. 1985. Simple versus complex carbohydrate use in the diabetic diet. Ann. Rev.Nutr. 5:95-114.
- Mendeloff, A.I. 1987. Dietary fibre and gastro intestinal disease. Am.J.Clin.Nutr.45 (suppl):1267-70.
- Bingham, S.A. 1996. Epidemiology and mechanisms relating diet to risk of colorectal cancer. Nutrition Research Reviews. 9:197-239.
- Dwyer, J.T. 1988. Health aspects of vegetarian diets. Am.J.Clin.Nutr. 48:712-28. 40.Cummings, J.H., Bingham, S.A., Heaton, K.W. and Eastwood, M.A. 1992. Faecal weight, colon cancer risk, and dietary intake of nonstarch polysaccharides (dietary fibre). Gastroentorology. 103:1783-1789.
- World Health Organization. 1990. Diet , Nutrition and the Prevention of Chronic Disease (Technical Report Series no. 797). Geneva:WHO.
- Leeds, A.R., Ralphs, D.N.L., Ebied, F., Metz, G., Dilawari, J.B. 1981. Pectin in the dumping syndrome and plasma volume changes. Lancet 1:1075-8.
- Braaten, J.T., Wood, P.J., Scott, F.W., Riedel, K.D.,Poste, L.M. and Collins, M.W. 1991. Oat gum lowers glucose and insulin after an oral glucose load. Am.J.Clin. Nutr.53:1425-30.
- Meyer, J.H., Guy, G., Jehn, D. Taylor, I.L. 1988. Intragastric vs intraintestinal viscous polymers and glucose tolerance after liquid meals of glucose. Am.J.Clin.Nutr. 48:260-6.
- Jenkins, D.J.A., Wolever, T.M.S., Taylor, R.H. et al. 1980. Rate of digestion of foods and post prandial glycemia in normal and diabetic subjects. Br.Med.J. 2:14-7.
- Batey, I.L. 1982. Starch analysis using thermostable alpha-amylase. Starch/Staerke. 34:125-8.
- Kelsay, J.L.; C.W. Frazier; ES Prather; JJ Canary; WM Clark and AS Powell. 1988 Impact of variation in carbohydrate intake on mineral utilization by vegetarians. Am.J Clin Nutr. 48:875-9.